Vertebrogenic Low Back Pain
Discover the ins and outs of vertebrogenic low back pain, from its origins in spinal structures to effective treatment options tailored to your needs.

Low back pain is a common ailment affecting millions of people worldwide. Among the various types of back pain, vertebrogenic low back pain is particularly noteworthy due to its direct association with the vertebral components of the spine.
This comprehensive guide will delve into the intricacies of vertebrogenic low back pain, offering insights into its causes, symptoms, diagnosis, and treatment options.
Summary
- Vertebrogenic low back pain is a condition caused by disorders of the vertebral bodies or intervertebral discs.
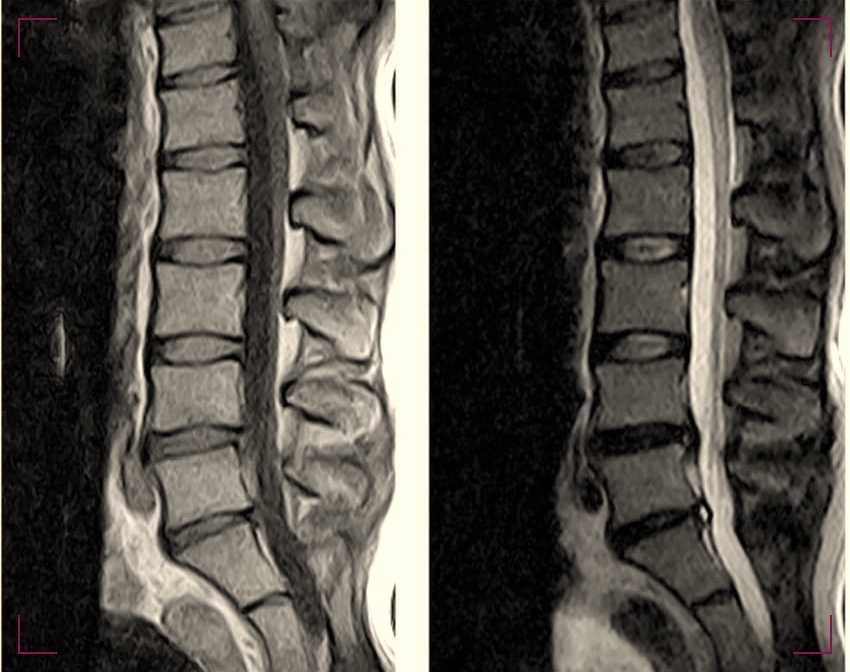
- Diagnosis often involves imaging techniques like MRI or CT scans to pinpoint the exact vertebral issue.
- Treatment can range from conservative methods like physical therapy to more invasive procedures such as surgery, depending on the severity.
What is Vertebrogenic Low Back Pain?
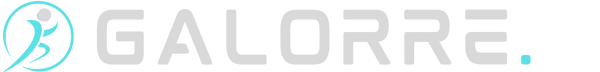
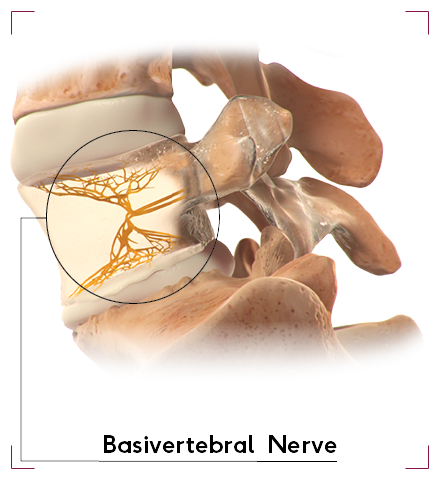
Vertebrogenic low back pain is a term used to describe pain that originates from the vertebral bodies or the intervertebral discs of the spine.
Unlike other forms of back pain that might be muscular or nerve-related, vertebrogenic pain is specifically tied to the bones and cartilage of the spinal column.
This type of pain can be chronic and debilitating, often impacting a person's ability to perform daily activities.
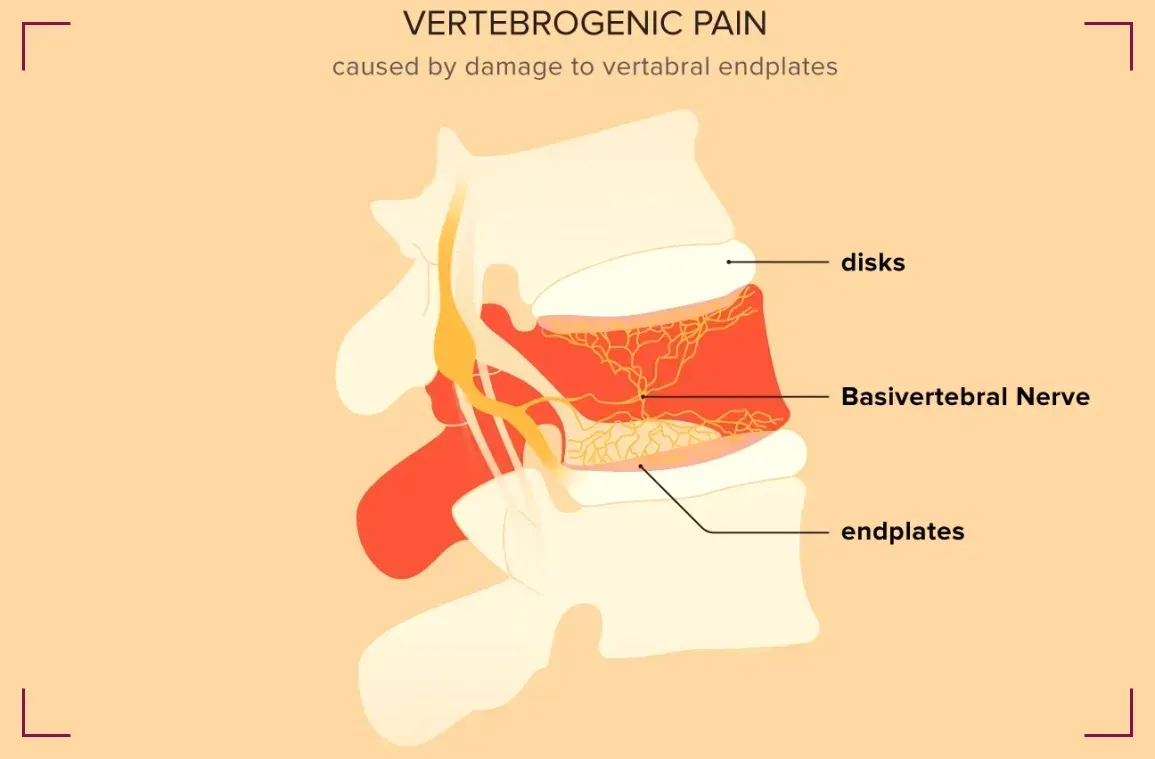
The spine is a complex structure made up of vertebrae, which are the bones stacked on top of each other, and discs, which act as cushions between them.
When these components are damaged or degenerate, they can cause pain that is classified as vertebrogenic.
The pain may be localized to the lower back or can radiate to other areas such as the buttocks or legs.
Causes and Risk Factors
Vertebrogenic low back pain can be attributed to a variety of causes. Degenerative disc disease is a common culprit, where the intervertebral discs lose hydration and elasticity, leading to reduced disc height and potential disc herniation.
Osteoarthritis can also play a role, as it leads to the breakdown of cartilage and the formation of bone spurs that can irritate spinal nerves.
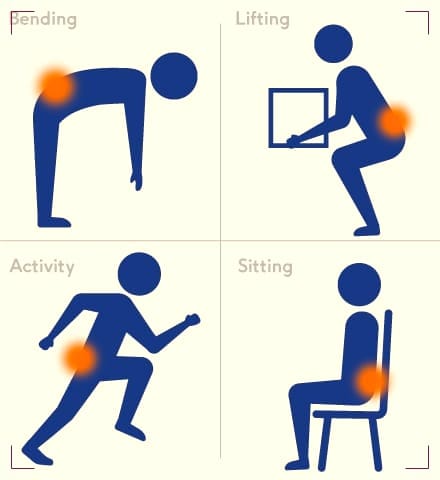
Risk factors for developing vertebrogenic low back pain include aging, which naturally leads to wear and tear on the spine, as well as lifestyle choices such as smoking, obesity, and occupations that require heavy lifting or prolonged sitting. Genetics may also predispose individuals to spinal disorders.
Symptoms
The primary symptom of vertebrogenic low back pain is, unsurprisingly, pain in the lower back region.
However, this pain can vary in nature; it might be a dull, aching sensation or a sharp, stabbing pain. It can also be accompanied by stiffness and reduced flexibility in the back.
In some cases, if the affected vertebral or disc issues impinge on spinal nerves, symptoms can extend beyond the back.
Patients may experience sciatica, characterized by pain, numbness, or tingling that radiates down the legs. Muscle weakness and difficulty with certain movements can also occur.
Diagnosis
To diagnose vertebrogenic low back pain, healthcare providers typically start with a thorough medical history and physical examination.
Imaging tests play a crucial role in confirming the diagnosis. Magnetic Resonance Imaging (MRI) is often the preferred method as it provides detailed images of both bone and soft tissues.
Computed Tomography (CT) scans and X-rays can also be utilized to assess the structural integrity of the vertebrae and discs.
In some cases, diagnostic injections such as facet joint injections or discography may be used to pinpoint the exact source of pain.
These procedures involve injecting a contrast dye into the suspected areas of the spine under imaging guidance to identify abnormalities.
Conservative Treatment Options
The initial approach to managing vertebrogenic low back pain typically involves conservative treatments.
Physical therapy is a cornerstone of non-invasive treatment, focusing on strengthening the muscles that support the spine and improving flexibility and posture.
Pain relief can also be achieved through medications such as non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants.
Lifestyle modifications are equally important. Patients are often advised to maintain a healthy weight, quit smoking, and adopt ergonomic practices in their daily activities. In some cases, chiropractic care or acupuncture may provide additional relief.
When Surgery Becomes Necessary
If conservative treatments fail to provide adequate relief, or if the vertebrogenic condition is severe, surgery may be considered.
Surgical options can range from minimally invasive procedures like microdiscectomy to more extensive surgeries such as spinal fusion.
The goal of surgery is to alleviate pain by correcting the underlying vertebral or disc problem.
The decision to undergo surgery is not taken lightly and involves a detailed discussion between the patient and their healthcare provider.
Factors such as the patient's overall health, the severity of symptoms, and the specific spinal condition will influence the choice of surgical intervention.
Alternative Therapies
Alternative therapies can sometimes provide additional comfort to those suffering from vertebrogenic low back pain.
Treatments such as massage therapy, yoga, and Pilates are known for their ability to reduce stress and improve the strength and flexibility of the back muscles.
However, it's important to consult with a healthcare provider before starting any new therapy to ensure it's appropriate for your specific condition.

Herbal supplements and nutritional strategies may also play a supportive role in managing back pain.
While these should not replace conventional treatments, they can be part of a comprehensive pain management plan.
Long-Term Management and Prevention
Managing vertebrogenic low back pain is often a long-term commitment. Patients may need to continue with physical therapy exercises and lifestyle adjustments to prevent the recurrence of pain.
Regular follow-up with healthcare providers is crucial to monitor the condition and make any necessary changes to the treatment plan.
Preventive measures can also be taken to reduce the risk of developing vertebrogenic low back pain.
These include maintaining good posture, engaging in regular physical activity, and using proper body mechanics when lifting heavy objects.
Summary
Vertebrogenic low back pain is a condition that arises from problems within the vertebral bodies or intervertebral discs. It can cause significant discomfort and limit a person's mobility and quality of life. Understanding the causes, symptoms, and available treatments is essential for those affected by this condition. With the right combination of conservative care, possible surgical intervention, and lifestyle changes, individuals can manage their pain and lead active lives.
FAQ Section
Q 1: What is vertebrogenic low back pain, and what causes it?
Vertebrogenic low back pain refers to pain originating from the vertebral structures of the spine, including the bones, joints, discs, and surrounding tissues. This type of back pain typically arises due to degenerative changes in the spine, such as disc herniation, spinal stenosis, or facet joint osteoarthritis.
These conditions can cause compression or irritation of spinal nerves, leading to symptoms such as localized back pain, radiating pain into the buttocks or legs (sciatica), stiffness, and reduced range of motion. Other contributing factors to vertebrogenic low back pain may include poor posture, repetitive movements, trauma, and genetic predispositions.
Effective management of vertebrogenic low back pain often involves a combination of conservative treatments and lifestyle modifications. These may include physical therapy exercises to improve spinal flexibility and strength, nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants to alleviate pain and inflammation, and ergonomic adjustments to reduce strain on the spine during daily activities.
In severe cases or when conservative measures fail to provide relief, invasive interventions such as epidural steroid injections or surgical procedures may be considered to address the underlying spinal pathology and alleviate symptoms.
Q 2: How is vertebrogenic low back pain diagnosed?
Diagnosing vertebrogenic low back pain typically involves a comprehensive evaluation by a healthcare professional, such as a primary care physician, orthopedic surgeon, or spine specialist.
The diagnostic process begins with a thorough medical history review, where the healthcare provider gathers information about the onset, duration, and characteristics of the back pain, as well as any relevant risk factors or previous treatments.
A physical examination follows, during which the provider assesses spinal alignment, range of motion, muscle strength, and neurological function. Imaging studies such as X-rays, MRI scans, or CT scans may be ordered to visualize the structures of the spine and identify any abnormalities or degenerative changes.
In some cases, additional diagnostic tests such as electromyography (EMG) or nerve conduction studies may be recommended to evaluate nerve function and rule out other potential causes of back pain.
Once a diagnosis of vertebrogenic low back pain is confirmed, the healthcare provider can develop an individualized treatment plan tailored to the patient's specific needs and preferences.
Q 3: What are the treatment options for Vertebrogenic low back pain?
Treatment options for vertebrogenic low back pain vary depending on the severity of symptoms, underlying spinal pathology, and individual patient factors.
Conservative measures are typically recommended as the initial approach and may include physical therapy, chiropractic care, acupuncture, and therapeutic exercises to improve spinal flexibility, strengthen supporting muscles, and alleviate pain.
Over-the-counter or prescription medications such as NSAIDs, muscle relaxants, or analgesics may be prescribed to manage pain and inflammation. In cases where conservative treatments fail to provide adequate relief, more invasive interventions may be considered.
These may include epidural steroid injections to reduce inflammation and alleviate nerve compression, radiofrequency ablation to disrupt pain signals from affected nerves, or minimally invasive spine surgery to address structural abnormalities such as herniated discs or spinal stenosis.
Patients need to work closely with their healthcare providers to develop a comprehensive treatment plan that addresses their specific needs and goals while minimizing risks and maximizing outcomes. Additionally, lifestyle modifications such as maintaining a healthy weight, practicing good posture, and engaging in regular exercise can help prevent recurrent episodes of vertebrogenic low back pain and promote long-term spinal health.