Understanding Septic Arthritis Lactate
Explore the significance of timely lactate measurements in shaping a targeted and effective approach to managing septic arthritis and mitigating the risk of systemic complications.
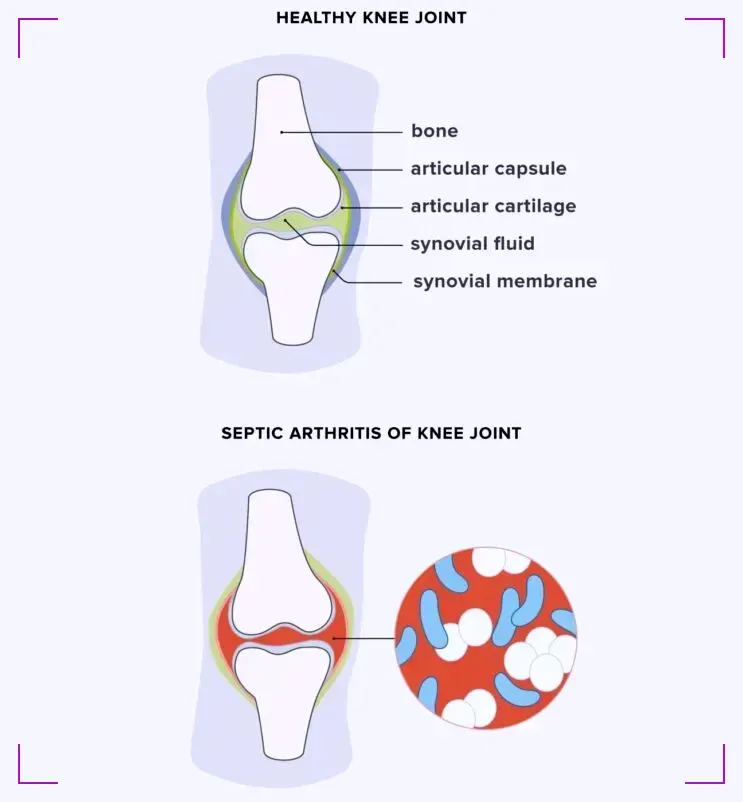
Septic arthritis, an intense and serious condition, occurs when a joint becomes infected, leading to severe pain, swelling, and difficulty in movement.
Among the various biomarkers for diagnosing this condition, lactate levels have emerged as a significant indicator. The condition is often diagnosed through blood tests. The treatment for septic arthritis is primarily based on the severity of the condition.
This article delves into the role of septic arthritis lactate, exploring its importance in diagnosis and treatment.
Key Takeaways
- Septic arthritis lactate is a critical biomarker in diagnosing septic arthritis, a painful joint infection.
- Early detection and treatment of septic arthritis are crucial to prevent joint damage and systemic complications.
What is Septic Arthritis?
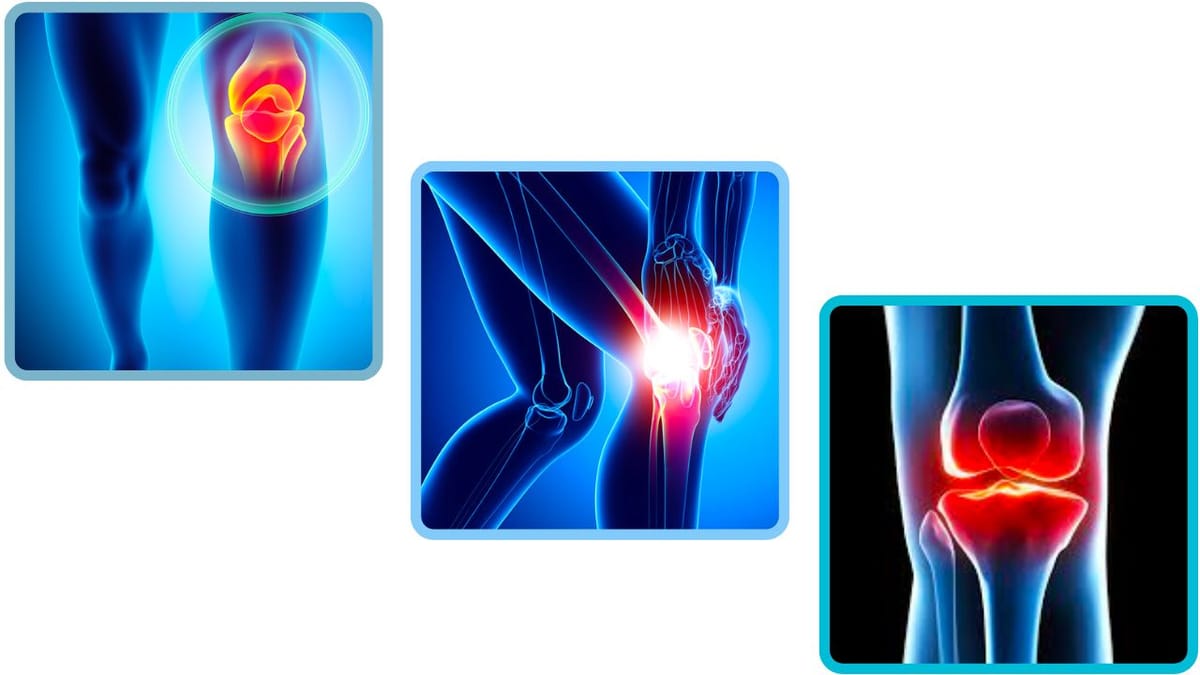
Septic arthritis, also known as infectious arthritis, is a serious medical condition characterized by the inflammation of a joint due to the presence of an infection. This type of arthritis occurs when bacteria, viruses, or fungi invade a joint, leading to the accumulation of inflammatory cells and causing pain, swelling, and decreased joint mobility.
Septic arthritis commonly affects large joints such as the knee, hip, or shoulder. The infection can enter the joint through various means, including the bloodstream (hematogenous spread) or direct extension from nearby tissues.
Individuals with compromised immune systems, pre-existing joint conditions, or those who have recently undergone joint surgery are at a higher risk of developing septic arthritis. Prompt diagnosis and treatment are essential to prevent long-term joint damage and systemic complications.
Treatment typically involves antibiotics and, in some cases, drainage of the infected joint fluid. Septic arthritis requires immediate medical attention to minimize the risk of irreversible joint damage and improve overall outcomes.
Lactate in Septic Arthritis
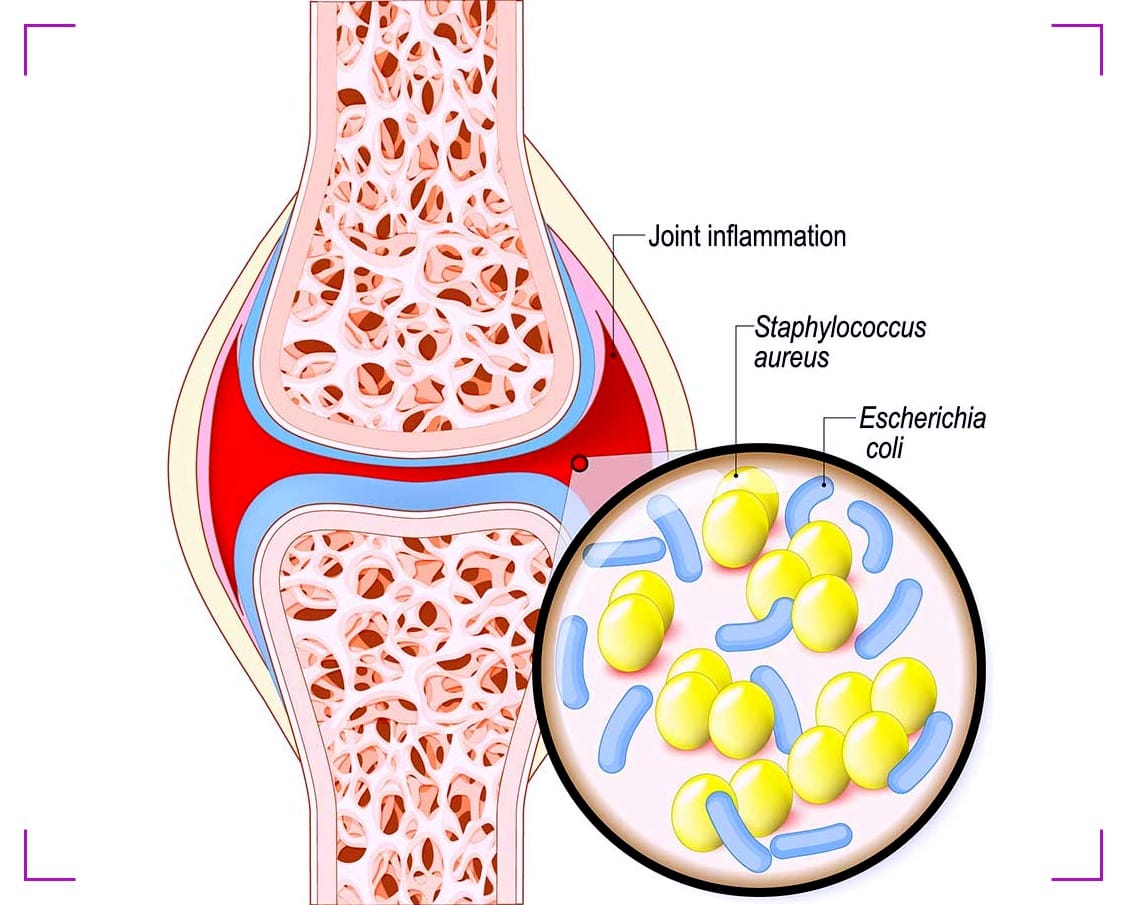
Lactate in septic arthritis is significant as it serves as a key biomarker that reflects the metabolic state of the affected tissues and helps gauge the severity of the infection.
Lactate is a byproduct of anaerobic metabolism, and its elevation in the context of septic arthritis indicates an insufficient supply of oxygen to the tissues, known as tissue hypoperfusion.
When an infection, such as septic arthritis, is present, the body's response includes an increase in lactate production due to impaired oxygen delivery and utilization in the affected joint.
Monitoring lactate levels is crucial in assessing the extent of tissue damage and systemic involvement. Persistently elevated lactate levels may suggest the presence of sepsis, a severe and life-threatening condition that can arise from the spread of infection.
In septic arthritis, elevated lactate levels guide healthcare providers in making informed decisions regarding the urgency and intensity of treatment. Serial measurements of lactate levels are conducted to track changes over time, helping healthcare professionals evaluate the effectiveness of interventions and make adjustments to the treatment plan as needed.
The role of lactate in septic arthritis management is integral, providing valuable insights into the metabolic status of the affected joint and guiding the healthcare team in optimizing patient care.
Diagnosing Septic Arthritis
The diagnosis of septic arthritis involves a combination of clinical evaluation, imaging studies, and laboratory tests to identify the presence of an infection within a joint. The following steps are typically taken in the diagnostic process:
- Clinical Assessment
Healthcare providers conduct a thorough physical examination to assess the affected joint. They look for signs of inflammation, such as swelling, redness, and warmth, and evaluate the range of motion. The patient's medical history, including recent infections, joint conditions, or surgeries, is also considered. - Joint Aspiration (Arthrocentesis)
Joint aspiration is a crucial diagnostic procedure where a needle is inserted into the affected joint to collect a sample of synovial fluid. This fluid is then sent to the laboratory for analysis. In septic arthritis, the synovial fluid is often cloudy and contains more white blood cells, and microbial cultures may reveal the presence of bacteria. - Laboratory Tests
Blood tests, including complete blood count (CBC) and inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), are conducted to assess the overall inflammatory response in the body. Elevated levels of these markers can indicate the presence of an infection. - Imaging Studies
Imaging, such as X-rays and magnetic resonance imaging (MRI), may be employed to visualize the joint and assess for any structural damage. While X-rays are useful for detecting bone abnormalities, an MRI provides detailed images of soft tissues and can help confirm the diagnosis. - Microbial Cultures
Microbial cultures from the synovial fluid obtained through joint aspiration are crucial for identifying the specific microorganism causing the infection. This information is essential for tailoring appropriate antibiotic treatment. - Additional Tests
Depending on the clinical presentation, additional tests may be performed, such as blood cultures or tests to rule out other potential causes of joint inflammation.
A prompt and accurate diagnosis is crucial in septic arthritis to initiate timely and targeted treatment, minimizing the risk of joint damage and systemic complications.
The comprehensive diagnostic process often involves coordination between healthcare professionals, including rheumatologists, orthopedic surgeons, and infectious disease specialists.
Septic Arthritis Lactate: A Biomarker for Infection
Lactate levels in the synovial fluid have been studied as a potential biomarker for septic arthritis. High lactate levels in the joint fluid may indicate an ongoing infection and the need for immediate intervention.

This biomarker helps differentiate septic arthritis from other conditions that cause joint inflammation, such as gout or rheumatoid arthritis.
Treatment Strategies
The treatment of septic arthritis involves a comprehensive strategy aimed at eradicating the infection, alleviating symptoms, and preventing long-term joint damage.
One of the primary pillars of treatment is the prompt initiation of antibiotic therapy. Intravenous administration of broad-spectrum antibiotics is initiated immediately to cover a spectrum of potential pathogens.
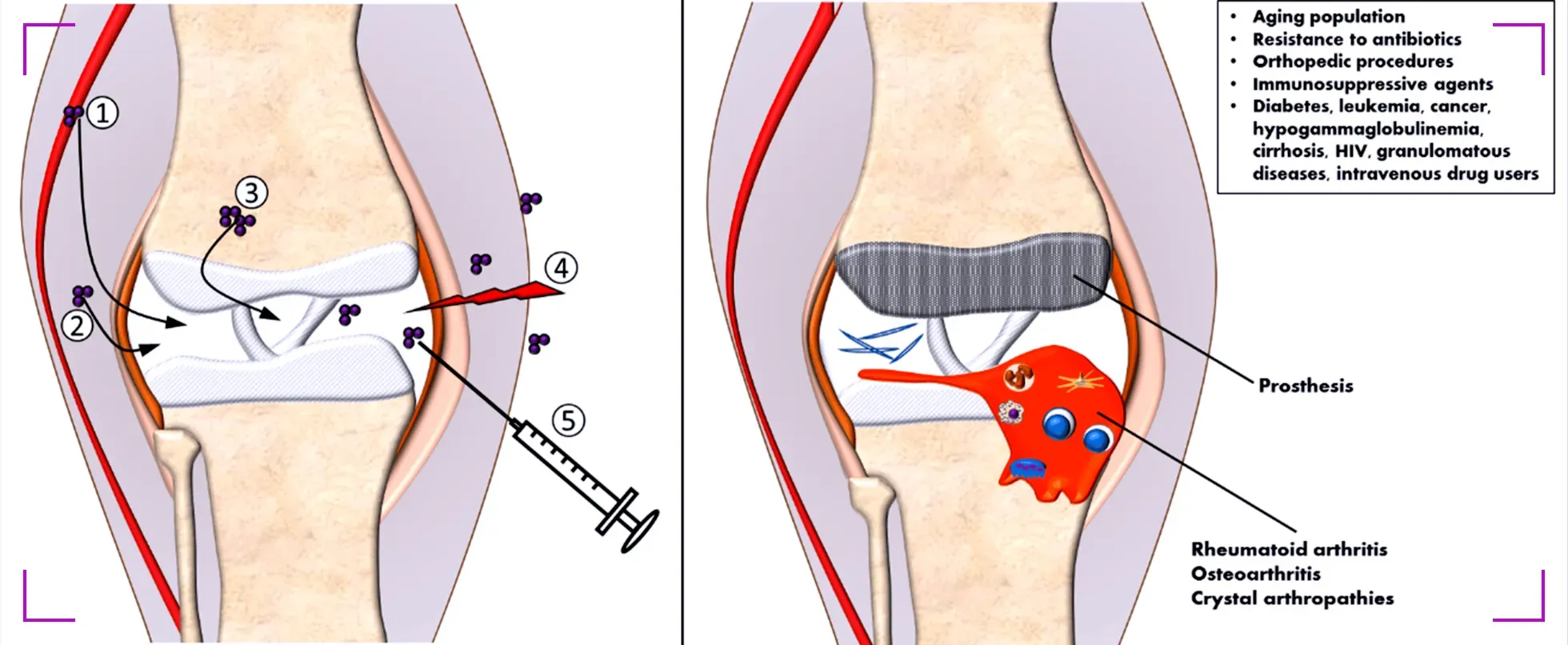
The choice of antibiotics is later refined based on the results of synovial fluid cultures, which identify the specific microorganism causing the infection. This targeted approach helps ensure effective and tailored treatment.
In conjunction with antibiotic therapy, joint aspiration is a crucial procedure. It involves removing synovial fluid from the infected joint to reduce intra-articular pressure and eliminate purulent material.
Surgical drainage may be necessary in cases where there is a significant accumulation of pus within the joint. These interventions not only contribute to the eradication of the infection but also aid in alleviating pain and inflammation.
Pain management is another integral aspect of septic arthritis treatment. Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen may be prescribed to relieve pain and reduce inflammation.
Early Detection
Early detection of septic arthritis is critical to prevent joint destruction and systemic spread of the infection.

Recognizing the signs and symptoms, along with measuring septic arthritis lactate levels, can lead to prompt treatment and a better prognosis for the patient.
Monitoring Lactate Levels During Recovery
As the patient undergoes treatment for septic arthritis, monitoring lactate levels can provide insights into the infection's progression or resolution.
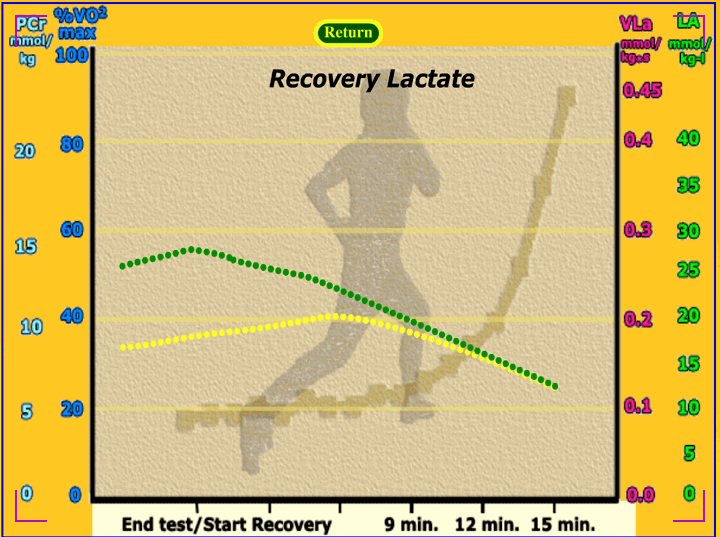
A decrease in lactate levels typically indicates a positive response to treatment, while persistently high levels may suggest the need for further intervention.
Preventing Septic Arthritis
While not all cases of septic arthritis can be prevented, understanding risk factors and practicing good hygiene can reduce the likelihood of developing the infection.
Prompt treatment of wounds and infections elsewhere in the body can also help prevent the spread to the joints.
Summary
Septic arthritis is a serious joint infection that requires prompt diagnosis and treatment. Lactate levels, both in the blood and synovial fluid, serve as a crucial biomarker for diagnosing the condition and monitoring treatment efficacy. Early detection, accurate diagnosis, and effective treatment strategies are essential to prevent long-term damage and complications. Understanding the role of septic arthritis lactate can significantly impact patient care and outcomes.
FAQ Section
Q 1: What Is the Significance of Lactate Levels in Septic Arthritis?
Answer: Lactate levels play a crucial role in assessing the severity and prognosis of septic arthritis. Elevated lactate levels indicate tissue hypoperfusion and anaerobic metabolism, suggesting a potential systemic response to the infection.
In the context of septic arthritis, an increase in lactate levels may signal the presence of sepsis, a severe and life-threatening complication. Monitoring lactate levels aids healthcare providers in gauging the extent of tissue damage, guiding treatment decisions, and identifying patients at higher risk for systemic complications.
Regular lactate level assessments are integral in managing septic arthritis, informing healthcare professionals about the patient's response to treatment and guiding adjustments to the therapeutic approach if necessary.
Q 2: How Are Lactate Levels Measured in Septic Arthritis Diagnosis?
Answer: Lactate levels are typically measured through blood tests, specifically a serum lactate test. In septic arthritis diagnosis, obtaining a blood sample allows healthcare providers to assess lactate concentration in the bloodstream.
Elevated lactate levels suggest impaired oxygen delivery to tissues and increased anaerobic metabolism, pointing toward the severity of the infection. Serial lactate measurements may be conducted to track changes over time and gauge the effectiveness of treatment.
While elevated lactate levels are a concerning indicator, they provide valuable information for healthcare professionals to tailor interventions, closely monitor patients, and address any systemic complications that may arise during septic arthritis.
Q 3: How Do Elevated Lactate Levels Impact the Treatment Approach for Septic Arthritis?
Answer: Elevated lactate levels in septic arthritis necessitate a comprehensive and urgent treatment approach. Addressing the underlying infection is paramount, often requiring prompt administration of intravenous antibiotics to target the causative microorganisms.
Aggressive fluid resuscitation may be initiated to improve tissue perfusion and alleviate the systemic effects of sepsis. In severe cases, where systemic complications are evident, intensive care measures may be implemented to stabilize the patient.
Continuous monitoring of lactate levels guides healthcare providers in assessing the response to treatment. A persistent elevation may indicate inadequate control of the infection or the development of systemic complications, prompting a reassessment of the therapeutic strategy.
Timely and targeted interventions based on lactate levels are crucial in improving outcomes and reducing the risk of severe complications in individuals with septic arthritis.