Herniated Disc and Sciatica
From the causes of disc herniation to the characteristic symptoms of sciatica and available treatment options, unravel the essential insights to navigate this common spinal concern.

A herniated disc and sciatica are terms that often go hand in hand when discussing back pain and spinal issues. Understanding these conditions is crucial for those who suffer from back pain or are at risk of developing such problems.
A herniated disc is a condition in which the discs in the spine become damaged or herniated. This can cause severe pain and loss of function. On the other hand, Sciatica is a condition that occurs when the sciatic nerve is inflamed or irritated, causing pain, numbness, and tingling in the butt.
In this article, we'll:
- Explore herniated discs and sciatica, and their interconnection.
- Symptoms of Herniated Disc and Sciatica.
- Diagnosis, treatment options, and preventive measures.
What is a Herniated Disc?
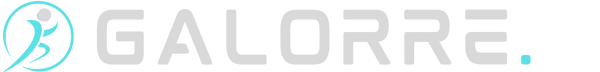
A herniated disc, also known as a slipped or ruptured disc, is a condition that occurs when the soft, gel-like center of a spinal disc protrudes through a tear or weakness in the tough outer layer.
These discs act as cushions between the vertebrae, providing flexibility, and shock absorption, and allowing smooth movement of the spine.
When a disc herniates, it can put pressure on nearby nerves, leading to various symptoms such as pain, numbness, or weakness in the affected area.
The condition is often associated with the natural aging process and wear and tear on the spine. As people age, spinal discs lose water content and become less flexible, making them more susceptible to herniation.
However, herniated discs can also result from injuries, trauma, or repetitive strain on the spine.
The symptoms and severity of a herniated disc can vary depending on its location and the extent of nerve compression.
While many people with herniated discs experience no symptoms or mild discomfort, others may require medical intervention to manage pain and improve function.
Connection Between Herniated Disc and Sciatica
The connection between a herniated disc and sciatica is rooted in the intricate interplay between spinal anatomy and nerve compression. A herniated disc occurs when the soft, gel-like material inside a spinal disc protrudes through its tough outer layer.
These discs serve as cushions between vertebrae, providing flexibility and shock absorption. However, when a disc herniates, the displaced material can impinge on adjacent nerve roots, including those constituting the sciatic nerve.
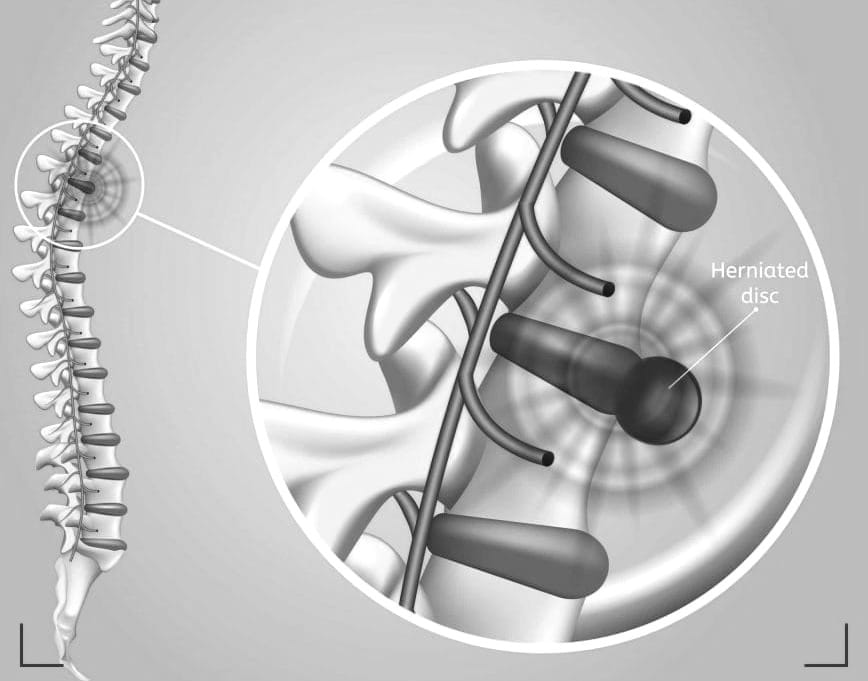
Sciatica, a condition characterized by pain, tingling, and numbness along the sciatic nerve's pathway, often finds its origin in herniated discs.
The location of the herniated disc determines which nerve roots are affected and consequently shapes the distribution of sciatic symptoms.

Typically, the pain begins in the lower back or buttocks and radiates down the back of the leg, sometimes extending to the foot.
While a herniated disc is a prevalent cause of sciatica, it's important to recognize that other spinal conditions, such as spinal stenosis or degenerative disc disease, can also lead to sciatic nerve compression.
Therefore, a comprehensive evaluation is essential to pinpoint the specific cause and guide an effective treatment approach.
In managing sciatica associated with a herniated disc, treatment strategies aim to address the underlying issue and alleviate symptoms.
Conservative measures, including rest, physical therapy, and pain medication, are often employed. In some cases, epidural steroid injections may be recommended to reduce inflammation around the affected nerve roots.
Surgical interventions, such as discectomy or microdiscectomy, may be considered if conservative measures prove insufficient.
Symptoms of Herniated Disc
Localized Back Pain
Pain in herniated disc area, often in the lower back. The pain may be intermittent or constant.
Radiating Pain
Pain radiates to other parts of the body, depending on the location of the herniated disc. For example, if in the lumbar spine, pain may radiate down the leg.
Numbness and Tingling
Sensations of numbness or tingling in the affected area, potentially extending to the extremities served by the compressed nerve.
Muscle Weakness
Weakness in muscles controlled by the affected nerve leads to difficulties in movement or coordination.
Changes in Reflexes
Altered reflexes, such as diminished knee jerk reflex, are associated with nerve compression.
Worsening Pain with Movement
Increased pain during certain movements, such as bending, lifting, or twisting.
Symptoms of Sciatica (Resulting from Herniated Disc)
Pain along the Sciatic Nerve Pathway
Pain that starts in the lower back or buttocks and radiates down the back of the leg, following the path of the sciatic nerve.
Burning or Shooting Pain
Intense, burning, or shooting pain that may extend from the buttocks to the foot.
Tingling and Numbness
Tingling sensations or numbness along the sciatic nerve, are often felt in the leg or foot.
Muscle Weakness
Weakness in the leg or foot muscles impacts mobility and strength.
Aggravation with Certain Activities
Exacerbation of symptoms with activities like sitting for prolonged periods, standing, or sudden movements.
Difficulty with Foot Movement
Difficulty moving the foot or toes, especially in severe cases.
Diagnosis
Diagnosing a herniated disc typically involves a comprehensive evaluation by a healthcare professional.
The process often begins with a thorough medical history review, where the patient provides information about symptoms, the onset of pain, and any factors that may exacerbate or alleviate discomfort.
A physical examination is conducted to assess reflexes, muscle strength, and areas of tenderness.
Imaging studies, such as X-rays, may be initially ordered to rule out other potential causes of back pain and to visualize the overall spinal structure.

However, since X-rays do not capture soft tissues like spinal discs, more advanced imaging tests like magnetic resonance imaging (MRI) or computed tomography (CT) scans are often employed for a detailed view of the spinal discs.
Whereas the diagnosis of sciatica associated with a herniated disc involves a similar comprehensive approach.
The healthcare provider considers the patient's medical history and conducts a physical examination, paying specific attention to the distribution of pain, muscle weakness, and any sensory changes.
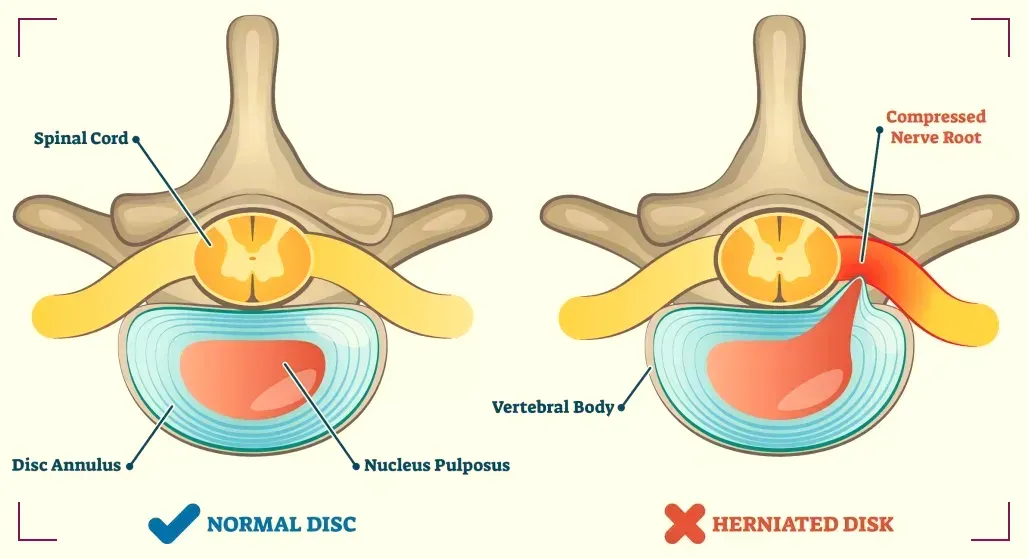
Imaging studies, particularly MRI, play a crucial role in confirming the presence of a herniated disc and its impact on the sciatic nerve.
The MRI provides detailed images of the spine, helping visualize the location and size of the herniation. This information is vital for determining the best course of treatment.
Surgical Interventions & Non-Surgical Treatment Options
Surgery might be considered when conservative treatments fail and the pain is disabling.
The most common surgical procedure for a herniated disc is a microdiscectomy, which involves removing the portion of the disc that is pressing on the sciatic nerve.
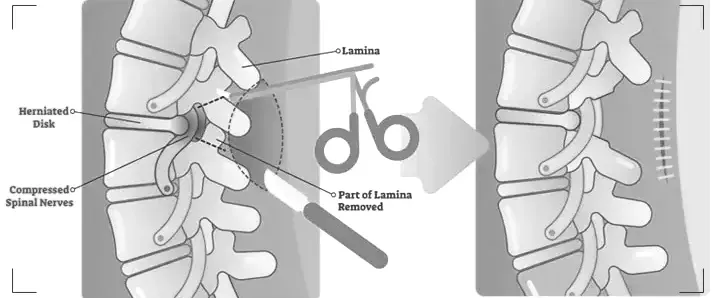
Another option is a laminectomy, where a section of the bone that covers the spinal canal is removed to relieve pressure.
The good news is that most people with a herniated disc and sciatica can find relief without surgery.
Treatment usually involves a combination of pain relief and physical therapy. Medications like NSAIDs, oral steroids, or muscle relaxants may be prescribed to manage pain and inflammation.
Physical therapy can help strengthen the back muscles, improve flexibility, and correct posture.
Lifestyle Changes, Home Remedies & Alternative Therapies
Making lifestyle changes can help manage the symptoms of a herniated disc and sciatica.
Maintaining a healthy weight, practicing good posture, and engaging in regular, low-impact exercise can reduce the strain on your spine.
Home remedies like applying heat or cold packs to the affected areas can also provide temporary relief.
Some people find relief from herniated disc and sciatica symptoms through alternative therapies.
Acupuncture, chiropractic adjustments, and massage therapy are popular options. While these treatments can provide temporary relief, it's important to discuss them with your doctor to ensure they're appropriate for your specific condition.

Preventive Measures
Preventing herniated discs involves maintaining a healthy spine. This can be achieved through regular exercise, maintaining good posture, especially when sitting for long periods, and using proper body mechanics when lifting heavy objects.

Additionally, quitting smoking can improve disc health, as nicotine has been shown to reduce blood flow to the discs.
Summary
FAQ Section
Q 1: What Causes a Herniated Disc and How Does It Lead to Sciatica?
Answer: A herniated disc is often a result of wear and tear on the spine, primarily associated with the natural aging process. As we age, spinal discs lose water content, becoming less flexible and more prone to herniation.
Additionally, injuries, trauma, or repetitive strain on the spine can contribute to disc herniation. When a disc herniates, the soft inner material protrudes through a tear in the outer layer, potentially pressing on adjacent nerve roots.
This compression, particularly on the sciatic nerve—the longest nerve in the body—gives rise to a condition known as sciatica. Sciatica manifests as pain, tingling, and numbness along the path of the sciatic nerve, often extending from the lower back down the back of the leg.
The connection between a herniated disc and sciatica lies in the impact of the displaced disc material on the sciatic nerve, leading to characteristic symptoms.
Q 2: What Are the Common Symptoms of Sciatica Caused by a Herniated Disc?
Answer: Sciatica resulting from a herniated disc presents with distinct symptoms. Individuals may experience sharp, shooting pain that originates in the lower back or buttocks and radiates down the leg.
This pain can be intense and may be accompanied by a burning or tingling sensation. Numbness along the sciatic nerve pathway, weakness in the leg or foot muscles, and changes in reflexes are also common indicators of sciatica.
The severity and combination of symptoms can vary, but they are often exacerbated by certain activities, such as prolonged sitting or sudden movements.
Understanding these characteristic symptoms is crucial for recognizing sciatica and seeking timely medical attention for an accurate diagnosis and appropriate treatment.
Q 3: What Treatment Options Are Available for Herniated Disc-Induced Sciatica?
Answer: The treatment of sciatica caused by a herniated disc typically begins with conservative measures. Rest, physical therapy, and pain medication are commonly employed to alleviate symptoms and promote recovery.
Epidural steroid injections may be recommended to reduce inflammation around the affected nerve roots. In cases where conservative treatments prove insufficient, surgical interventions like discectomy or microdiscectomy may be considered to address the herniated disc directly.
The choice of treatment depends on factors such as the severity of symptoms, the location of the herniated disc, and individual health considerations.
Seeking prompt medical attention and adhering to a tailored treatment plan are essential for effectively managing herniated disc-induced sciatica and improving long-term outcomes.