Herniated Disc & Their Impact on Daily Life
Explore measures or consider surgical intervention, understanding the nuances of herniated discs empowers individuals to navigate their path to relief and recovery with informed choices.

A herniated disc can be a source of significant discomfort and disability for many individuals. This condition, which affects the spine, can lead to pain, numbness, and a reduction in quality of life.
This comprehensive guide will explore what a herniated disc is, its causes, symptoms, and the various treatment options available.
Summary
- A herniated disc occurs when the soft center of a spinal disc pushes through a crack in the tougher exterior casing.
- Symptoms can include pain, numbness, and weakness in the affected area and the limbs.
- Treatment options range from conservative methods like physical therapy to surgical interventions in severe cases.
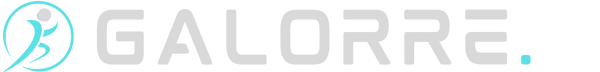
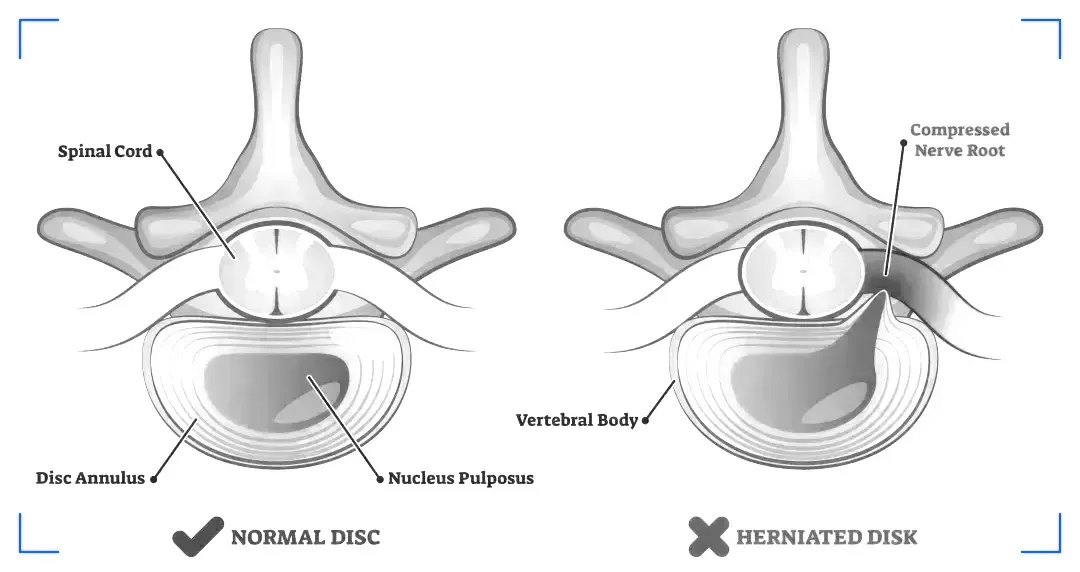
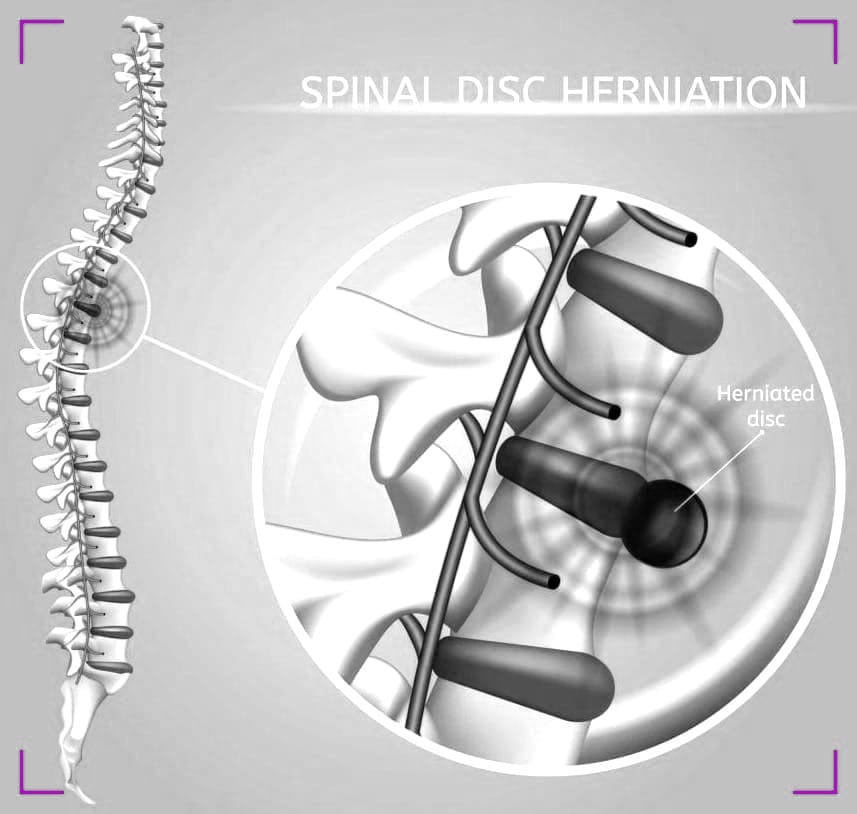
What is a Herniated Disc?
A herniated disc, also known as a slipped or ruptured disc, occurs when the inner gel-like core of a spinal disc pushes out through a tear in the disc's outer ring. This can irritate nearby nerves and result in pain, numbness, or weakness in an arm or leg.
Not everyone with a herniated disc, however, experiences symptoms, and for some, the condition may not require surgical treatment.
The spine is made up of a series of bones called vertebrae, and between each vertebra is a disc that acts as a cushion and provides flexibility to the spine.
These discs can deteriorate or become damaged due to various factors, leading to a herniation.
Understanding the anatomy of the spine is crucial in comprehending how a herniated disc can affect your body.
Causes
Herniated discs are most commonly the result of gradual, age-related wear and tear called disc degeneration.
Our spinal discs lose some of their water content as we age, making them less flexible and more prone to tearing or rupturing with even a minor strain or twist.
Most people can't pinpoint the exact cause of their herniated disc. Sometimes, using your back muscles instead of your leg and thigh muscles to lift heavy objects can lead to a herniated disc, as can twisting and turning while lifting.
Rarely, a traumatic event such as a fall or a blow to the back can cause a herniated disc.
Symptoms
The symptoms of a herniated disc can vary depending on the location of the affected disc and the nerves involved. Common symptoms include:
- Pain: Sharp or dull pain that may radiate along the path of the affected nerve. For example, a herniated disc in the lower back may cause sciatic pain that travels down the leg.
- Numbness and Tingling: Sensations of numbness or tingling, often felt in the area served by the affected nerve. This can lead to a "pins and needles" sensation.
- Muscle Weakness: Weakness in the muscles controlled by the affected nerves. This weakness may impact mobility and coordination.
- Changes in Reflexes: Reflexes controlled by the affected nerves may be altered. For instance, the knee-jerk reflex may be diminished.
- Bowel or Bladder Dysfunction: In rare cases, a severe herniated disc in the lower back may cause bowel or bladder dysfunction. This requires immediate medical attention.

It's essential to note that not everyone with a herniated disc experiences the same symptoms, and some individuals may be asymptomatic.
If you suspect a herniated disc or are experiencing persistent symptoms, it's crucial to consult with a healthcare professional for an accurate diagnosis and appropriate management.
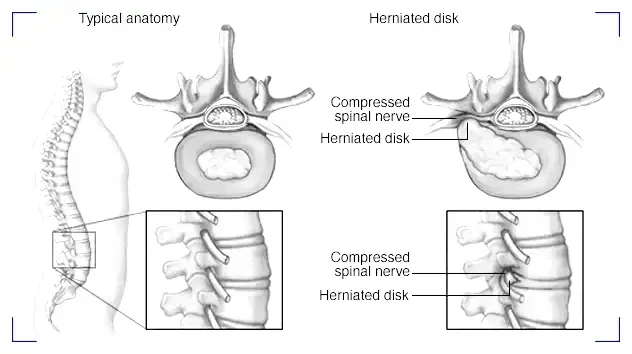
Diagnosis
To diagnose a herniated disc, a physician will perform a physical exam and may order imaging tests such as MRI or CT scans to confirm the diagnosis and to rule out other conditions.
During the physical exam, your doctor will check your back for tenderness, as well as your reflexes, muscle strength, walking ability, and sensation in your limbs.
An MRI is the most common imaging test used to diagnose a herniated disc in the spine.
Non-Surgical Treatment Options
The majority of herniated disc patients respond well to non-surgical treatment options.
These may include rest, pain medications, physical therapy, and epidural steroid injections.
Physical therapy can play a pivotal role in the recovery process, providing exercises that strengthen the muscles supporting the spine and reduce the pressure on the herniated disc.
Surgical Interventions
Surgical interventions for a herniated disc are considered when conservative treatments have not provided relief, and the symptoms are severe or progressive. Here are common surgical options:
- Discectomy:
In a discectomy, the surgeon removes a portion of the herniated disc that is pressing on the nerve. Relieve pressure on the nerve, reducing pain and improving symptoms.
- Microdiscectomy:
Similar to a discectomy but performed with a smaller incision and a microscope or magnifying lens for enhanced precision. Minimize tissue damage, reduce recovery time, and target the herniated disc with greater accuracy.
- Laminectomy:
In a laminectomy, part of the lamina (a bony plate) is removed to create more space and relieve pressure on the nerves. Increase the spinal canal's capacity and alleviate compression on the nerve roots.
- Spinal Fusion:
Spinal fusion involves fusing two or more vertebrae using bone grafts or implants to stabilize the spine. Provide stability to the spine and prevent movement between vertebrae, especially after removing a disc.
- Artificial Disc Replacement:
An artificial disc is inserted to replace the herniated disc, allowing for natural movement. Maintain spinal flexibility while addressing the damaged disc.
- Endoscopic Discectomy:
A minimally invasive technique using an endoscope to visualize and remove the herniated disc. Reduce tissue damage, minimize scarring, and expedite recovery.
Lifestyle Adjustments and Home Remedies
In addition to medical treatments, certain lifestyle adjustments and home remedies can help manage the symptoms of a herniated disc.
These include practicing good posture, using proper body mechanics, engaging in regular low-impact exercise, and applying heat or cold therapy to the affected area. Maintaining a healthy weight can also reduce the strain on the spine.
Alternative Therapies
Some individuals find relief from herniated disc symptoms through alternative therapies such as acupuncture, chiropractic treatment, and massage therapy.

While these treatments may provide temporary relief, it's important to consult a healthcare professional before starting any alternative therapies to ensure they are safe and appropriate for your condition.
Prevention Strategies
While it's not always possible to prevent a herniated disc, there are steps you can take to reduce your risk.
These include maintaining a healthy weight, staying active, avoiding tobacco, lifting objects correctly, and ensuring that you get enough calcium and vitamin D to keep your bones strong.
Regular exercise that focuses on strengthening the core muscles can also help stabilize and support the spine.
Summary
A herniated disc is a common condition that can cause pain, numbness, and weakness. While it can be debilitating, most people find relief through non-surgical treatments such as medication, physical therapy, and lifestyle changes. Surgery is reserved for those who do not respond to conservative treatments or who have significant nerve impairment. By understanding the causes, symptoms, and treatment options, individuals can better manage their condition and improve their quality of life.
FAQ Section
Q 1: What Causes a Herniated Disc?
A: A herniated disc, also known as a slipped or ruptured disc, is often caused by the natural aging process and wear and tear on the spine. The primary factors contributing to the development of a herniated disc include:
- Degeneration: Over time, the spinal discs lose water content and elasticity, making them more prone to degeneration. This natural aging process weakens the discs and increases the risk of herniation.
- Improper Lifting Techniques: Lifting heavy objects with improper techniques, especially when combined with twisting or turning motions, can exert excessive pressure on the spine and lead to disc herniation.
- Repetitive Strain: Repetitive movements or activities that involve straining the spine, such as improper bending or twisting, can contribute to the breakdown of disc material.
- Spinal Injury: Trauma or injury to the spine, such as a sudden fall or impact, can cause disc herniation. Accidents, sports injuries, or other physical traumas may result in a herniated disc.
- Genetic Factors: Some individuals may be genetically predisposed to conditions that affect the strength and integrity of spinal discs, increasing their susceptibility to herniation.
- Smoking: Smoking has been associated with an increased risk of disc degeneration. Nicotine and other substances in tobacco can impair blood flow to the spinal discs, affecting their health.
It's important to note that while these factors contribute to the development of a herniated disc, the condition can also occur without any apparent cause. Aging and degeneration remain primary contributors, and the risk tends to increase with advancing age.
Maintaining a healthy lifestyle, practicing proper body mechanics, and seeking prompt medical attention for spinal injuries can help reduce the risk of developing a herniated disc.
Q 2: What Are the Common Symptoms of a Herniated Disc?
A: The symptoms of a herniated disc can vary based on the location of the affected disc and the nerves involved. Common symptoms include:
Pain:
Sharp, shooting pain that may radiate along the path of the affected nerve. For example, a herniated disc in the lower back can cause sciatic pain radiating down the leg.
Numbness and Tingling:
Sensations of numbness or tingling, are often felt in the area served by the affected nerve. This can lead to a "pins and needles" sensation.
Muscle Weakness:
Weakness in the muscles controlled by the affected nerves. This weakness may impact mobility and coordination.
Changes in Reflexes:
Reflexes controlled by the affected nerves may be altered. For instance, the knee-jerk reflex may be diminished.
Bowel or Bladder Dysfunction:
In rare cases, a severe herniated disc in the lower back may cause bowel or bladder dysfunction. This requires immediate medical attention.
It's essential to note that not everyone with a herniated disc experiences the same symptoms, and some individuals may be asymptomatic. Additionally, symptoms may come and go, and their severity can vary.
If you suspect a herniated disc or are experiencing persistent symptoms, it's crucial to consult with a healthcare professional for an accurate diagnosis and appropriate management.
Q 3: What Treatment Options are Available for a Herniated Disc?
A: Treatment options for a herniated disc vary depending on the severity of symptoms and the individual's overall health. Common approaches include:
- Conservative Measures:
Rest: Adequate rest and avoiding activities that worsen symptoms.
Pain Medication: Over-the-counter or prescription pain relievers to manage pain and inflammation.
Physical Therapy: Targeted exercises to strengthen muscles, improve flexibility, and alleviate pressure on the affected disc.
- Epidural Steroid Injections:
Injections of corticosteroids into the affected area to reduce inflammation and provide temporary relief.
- Chiropractic Care:
Spinal adjustments and manipulations by a chiropractor to help alleviate pain and improve spinal function.
- Heat and Ice Therapy:
Application of heat or cold packs to the affected area for pain relief and inflammation reduction.
- Lifestyle Modifications:
It is adopting proper body mechanics, maintaining good posture, and avoiding activities that strain the spine.