Unraveling the Mysteries of Claudication - Causes, Symptoms & Solutions
From understanding its vascular origins to exploring effective management strategies, we delve into the world of claudication to empower individuals with insights for a healthier, more active life.

Claudication is a medical term that refers to pain or discomfort, usually in the legs, that occurs during physical activity and is a common symptom of peripheral artery disease (PAD). This condition is often a result of inadequate blood flow to the muscles, restricting their oxygen supply.
This condition can significantly impact one's quality of life, but with the right knowledge and management strategies, individuals can alleviate symptoms and improve their overall health.
In this article, we will delve into the causes, symptoms, and various treatment options available for individuals experiencing claudication.
Claudication
Claudication refers to muscle pain, cramping, or leg fatigue that occurs during physical activity such as walking and subsides with rest. This condition is typically caused by insufficient blood flow to the muscles, often due to peripheral artery disease.
PAD is a circulatory problem where narrowed arteries reduce blood flow to the limbs. When you walk or exercise, your leg muscles require increased blood flow; if the arteries cannot supply enough blood, you may feel pain or discomfort.
The pain from claudication can be described as aching, burning, or a sense of fatigue in the muscles. It most commonly affects the calves but can also occur in the buttocks, thighs, or feet.
The severity of the pain can vary, ranging from mild discomfort to severe pain that can hinder daily activities.
Symptoms
The hallmark symptom of claudication is leg pain that occurs during physical activity and is relieved by rest.
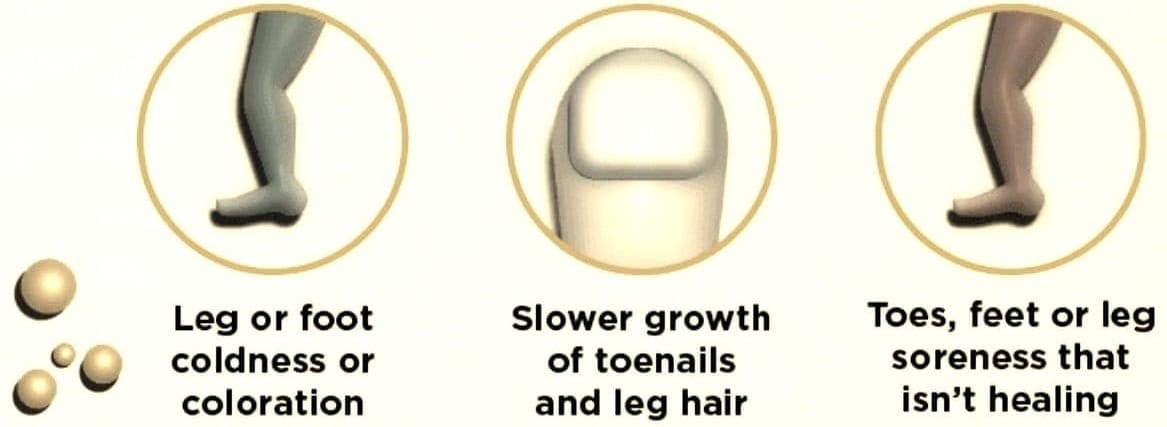
However, other signs and symptoms may include a feeling of heaviness in the legs, weakness, or numbness. In some cases, individuals may experience coldness in the lower leg or foot, particularly when compared with the other side.
It's important to note that claudication symptoms can be mistaken for other conditions such as arthritis or neuropathy.
Therefore, it is crucial to consult a healthcare professional for an accurate diagnosis if you experience any persistent leg pain, especially if it occurs during exercise and subsides with rest.
Causes
The primary cause of claudication is peripheral artery disease, which is often the result of atherosclerosis.
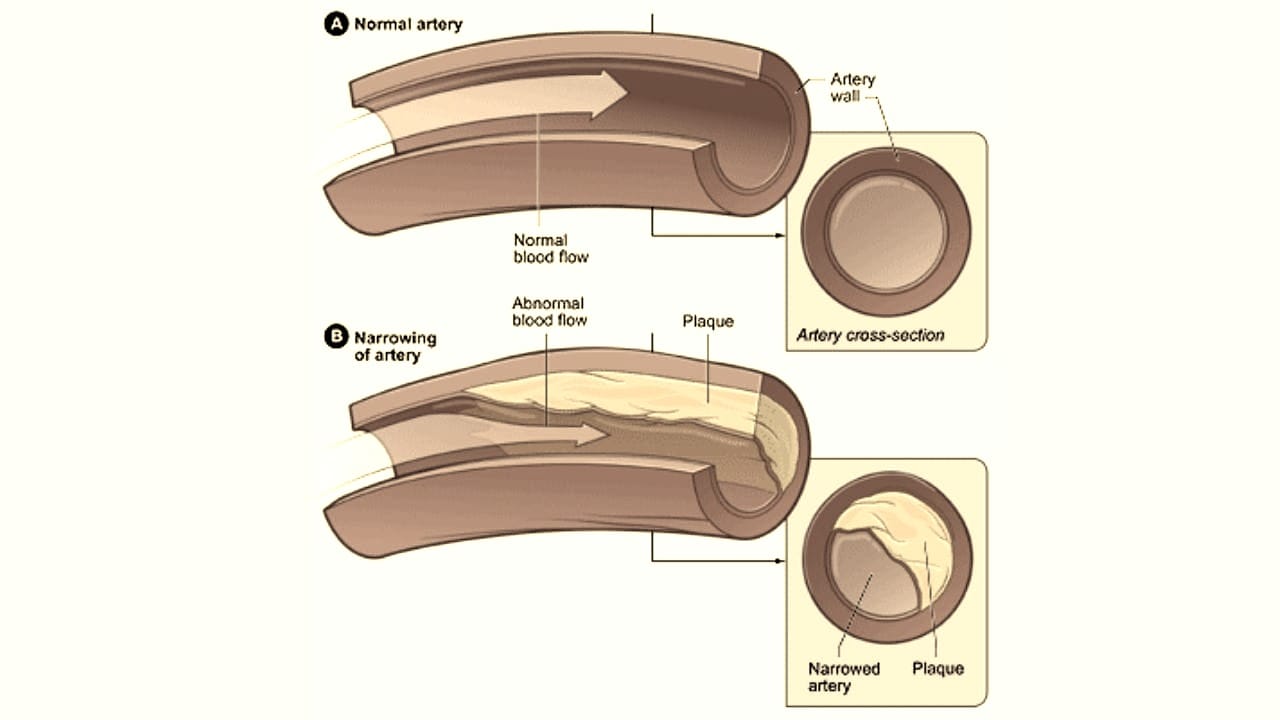
Atherosclerosis is the buildup of fatty deposits, or plaques, on the artery walls, which can reduce blood flow.
Risk Factors
Several risk factors can increase the likelihood of developing PAD and claudication, including smoking, diabetes, high blood pressure, high cholesterol, obesity, and a sedentary lifestyle.
Age is also a significant risk factor, as the incidence of PAD increases with age. A family history of PAD, heart disease, or stroke can predispose an individual to claudication. Understanding these risk factors is essential for prevention and early intervention.
Complications
Intermittent claudication itself is not directly life-threatening, it can indicate underlying vascular issues that may lead to complications.
Here are potential complications associated with claudication:
- Skin lesions that don't heal
- Death of muscle and skin tissues (gangrene)
- Amputation of a limb
Diagnosis
Diagnosing claudication typically involves a physical examination and a review of the patient's medical history and symptoms.
The ankle-brachial index (ABI) test is a common non-invasive test used to diagnose PAD.
It compares the blood pressure in the ankle with the blood pressure in the arm to determine how well blood flows.
Additional tests may include imaging studies such as Doppler ultrasound, magnetic resonance angiography (MRA), or computed tomography angiography (CTA) to visualize the blood flow in the arteries and pinpoint any blockages or narrowing.
Treatment Options
Treatment for claudication focuses on improving symptoms and stopping the progression of PAD. Lifestyle changes are often the first line of defense, including quitting smoking, engaging in regular exercise, and adopting a healthy diet.
Medications may also be prescribed to improve blood flow, such as antiplatelet agents or cholesterol-lowering drugs.
In more severe cases, medical procedures like angioplasty, stent placement, or bypass surgery may be necessary to restore proper blood flow to the affected limbs.
These treatments can significantly reduce symptoms and improve the ability to walk without pain.
Exercise
Exercise is a critical component in managing claudication. A supervised exercise program can help increase the distance you can walk without pain and improve cardiovascular health.

Walking is the most recommended form of exercise for individuals with claudication, as it encourages the development of small blood vessels that can bypass blockages.
It's essential to start slowly and gradually increase the duration and intensity of exercise under the guidance of a healthcare provider. Consistency in following an exercise regimen can significantly improve symptoms and quality of life.
Medications and Surgical Interventions
When lifestyle changes and exercise are not enough to manage claudication symptoms, medications may be prescribed.

These can include cilostazol or pentoxifylline, which can help improve blood flow and reduce symptoms.
Antiplatelet medications like aspirin or clopidogrel may also be recommended to prevent blood clots.
For those with severe PAD, surgical interventions such as angioplasty or bypass surgery may be necessary. These procedures can open up or bypass blocked arteries, restoring blood flow and reducing claudication symptoms.
Preventing Claudication
Preventing claudication starts with addressing the risk factors for peripheral artery disease.
This includes smoking cessation, maintaining a healthy weight, controlling blood sugar levels if diabetic, managing blood pressure and cholesterol, and staying physically active.
Regular check-ups with a healthcare provider can help detect early signs of PAD and claudication, allowing for timely intervention.
Educating oneself about claudication's risk factors and symptoms is also crucial for prevention and early treatment.
Summary
Claudication is a symptom of peripheral artery disease that can cause significant discomfort and limit mobility. Understanding the causes, recognizing the symptoms, and seeking timely medical intervention are key to managing this condition. With a combination of lifestyle changes, exercise, medications, and possibly surgical interventions, individuals with claudication can improve their symptoms and quality of life.
FAQ Section
Q: What is Claudication, and How Does It Differ from Everyday Leg Pain?
A: Claudication is a specific type of leg pain associated with poor blood flow, typically occurring during physical activity and alleviated with rest.
Unlike everyday leg pain, claudication is often caused by arterial insufficiency and manifests as cramping, tightness, or weakness, making it crucial to distinguish and address its underlying vascular component.
Q: What are the Common Causes and Risk Factors for Claudication?
A: Claudication is commonly caused by peripheral artery disease (PAD), where arteries that supply blood to the legs become narrowed or blocked. Smoking, diabetes, high blood pressure, and advanced age are significant risk factors.
Other causes may include atherosclerosis and blood vessel inflammation. Identifying and managing these risk factors is essential for preventing and treating claudication.
Q: How Can Claudication be Managed and Treated?
A: Claudication management often involves lifestyle modifications such as regular exercise, smoking cessation, and a heart-healthy diet. Medications to control risk factors, like cholesterol-lowering drugs, may be prescribed.
In more severe cases, medical procedures such as angioplasty or bypass surgery might be recommended. Supervised exercise programs tailored to individual capabilities can significantly improve symptoms and quality of life for those with claudication.