Are Sciatica and Shingles Related? Exploring the Connection
Understanding the differences is essential for accurate diagnosis, enabling individuals to navigate their symptoms effectively and seek timely medical attention.

Sciatica and shingles are two distinct medical conditions that can cause significant discomfort and pain. While they may seem unrelated at first glance, there are aspects of their manifestation that can lead to confusion and misdiagnosis.
This article aims to explore the relationship between sciatica and shingles, shedding light on their symptoms, causes, and treatments.
Key Takeaways:
- Sciatica and shingles are different conditions with overlapping symptoms, particularly pain.
- Shingles can sometimes lead to a complication called postherpetic neuralgia, which can mimic sciatica symptoms.
- Understanding the differences and similarities between sciatica and shingles is crucial for proper diagnosis and treatment.
What is Sciatica?
Sciatica is a term used to describe the pain that radiates along the path of the sciatic nerve, which extends from the lower back through the hips and buttocks and down each leg.
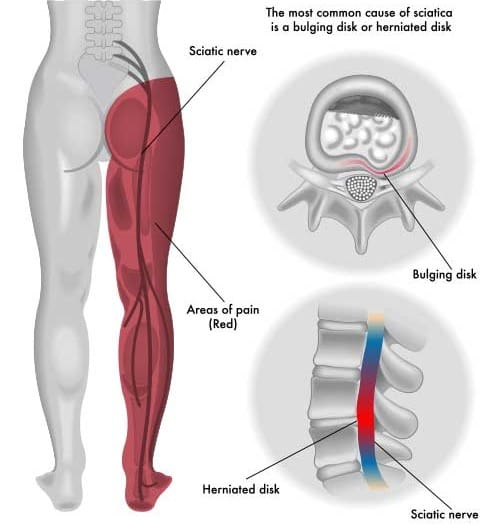
Typically, sciatica affects only one side of the body. A herniated disk often causes it, bone spurs on the spine, or narrowing of the spine (spinal stenosis) compressing part of the nerve.
This compression leads to inflammation, pain, and often some numbness in the affected leg.
The Nature of Shingles
Shingles, on the other hand, is caused by the varicella-zoster virus, the same virus that causes chickenpox.
After a person recovers from chickenpox, the virus can remain dormant in the body and reactivate years later, leading to shingles.

It is characterized by a painful rash that usually appears as a single stripe of blisters that wraps around either the left or the right side of the torso. Shingles can also affect the face and other body parts.
Symptoms of Sciatica
The hallmark symptom of sciatica is a sharp, shooting pain that makes it difficult to stand up or walk.
Symptoms can vary widely from a mild ache to a sharp, burning sensation or excruciating pain. Some people also experience muscle weakness, tingling, or numbness in the affected leg.
Typically, the discomfort is felt in a narrow segment of the body along the path of the sciatic nerve.
Identifying Shingles Symptoms
Shingles symptoms start with a tingling sensation or pain on one side of the body or face, followed by a red rash that develops a few days later.
The rash forms blisters that typically scab over in 7 to 10 days and clear up within 2 to 4 weeks.
Before the rash appears, people often experience pain, itching, or tingling in the area where the rash will develop. This can sometimes be confused with the pain of sciatica.
Causes of Sciatica
Sciatica is most commonly a result of a lumbar herniated disc directly pressing on the nerve.
Other causes include degenerative disc disease, isthmic spondylolisthesis, and spinal stenosis.
Risk Factors of Sciatica
Risk factors for developing sciatica include age, obesity, occupation, prolonged sitting, and diabetes.
Each of these factors can contribute to the nerve compression that leads to sciatica pain.
Shingles: Triggers and Risk Factors
Shingles is triggered by the reactivation of the varicella-zoster virus. Factors that can increase the risk of developing shingles include being older than 50, having certain diseases that weaken the immune system, undergoing cancer treatments, taking certain medications, and stress. Unlike sciatica, shingles are not caused by physical compression but by a viral infection.
Treatment Options for Sciatica
Treatment for sciatica typically involves non-operative methods such as physical therapy, anti-inflammatory medication, and hot or cold packs.
In some cases, doctors may recommend steroid injections or surgery if the pain is severe and does not improve with other treatments.
The goal of treatment is to relieve pain and address the underlying condition causing the nerve compression.
Managing Shingles and Postherpetic Neuralgia
The treatment for shingles includes antiviral medications, pain relievers, and corticosteroid injections to reduce inflammation and pain.
For ongoing nerve pain from shingles, known as postherpetic neuralgia, doctors may prescribe medications specifically for nerve pain, antidepressants, or topical agents.
Early treatment of shingles can help shorten the length of the infection and reduce the risk of complications.
Preventative Measures and Lifestyle Adjustments
Preventing sciatica involves regular exercise, proper posture, and ergonomic workstations.
Maintaining a healthy weight can also reduce the risk of developing sciatica. For shingles, the most effective prevention is vaccination.
The shingles vaccine is recommended for adults over 50 and can significantly reduce the risk of developing shingles and its complications.
Summary
FAQ Section
Q 1: Is There a Connection Between Sciatica and Shingles?
A: Sciatica and shingles are distinct conditions, but they can cause similar symptoms such as shooting pain, tingling, and numbness.
While sciatica originates from the irritation of the sciatic nerve, often due to a herniated disc, shingles are a viral infection caused by the varicella-zoster virus, leading to a painful rash.
Although different, both conditions can result in nerve-related discomfort.
Q 2: How Can I Differentiate Between Sciatica and Shingles?
A: Sciatica typically presents as pain radiating down the leg, often on one side, while shingles commonly manifest as a painful rash that follows a dermatome pattern.
Sciatica is primarily a nerve compression issue, while shingles is a viral infection affecting nerves. Consulting a healthcare professional for a thorough examination and appropriate tests is crucial for an accurate diagnosis.
Q 3: Can Shingles Lead to Sciatica or Exacerbate Existing Sciatic Nerve Pain?
A: While shingles and sciatica are distinct, shingles affecting nerves can, in rare cases, lead to postherpetic neuralgia, causing persistent nerve pain.
This lingering pain might resemble sciatic nerve pain. It's important to note that having had shingles does not directly cause sciatica.
If you experience new or worsening symptoms, seeking medical attention is crucial for proper evaluation and management.